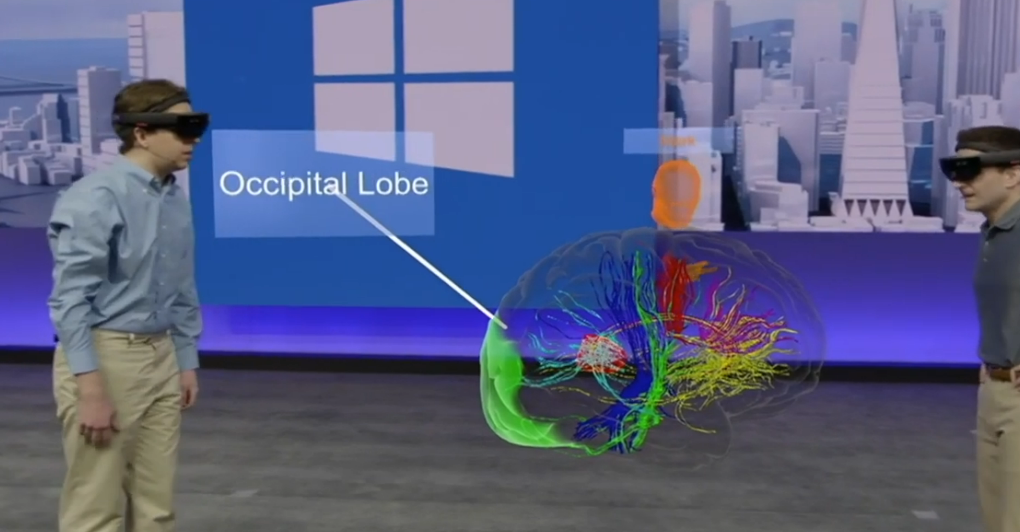
Virtual reality is quickly taking over as the beating heart of contemporary medical education. Instead of using static diagrams to learn anatomy, medical students now virtually walk through organs, tissues, and arteries to learn about the human body from the inside out. They are able to understand intricate systems that textbooks only allude to because the experience feels real.
Trainees at Harvard Medical School engage in simulated surgeries that replicate actual tension and timing. They are able to repeat processes, make mistakes with no repercussions, and precisely hone techniques. A Harvard Business Review study claims that surgical performance can be enhanced by up to 230% through VR-based training. This data shows that virtual training enhances experiential learning rather than replaces it.
In an incredibly clear analogy, Dr. Justin Pottle of the National Institutes of Health describes this change: “VR has become the stethoscope of education — not just listening, but immersing.” His observation sums up why educational institutions are rushing to incorporate virtual tools into their curricula. Students now live procedures rather than merely learning them.
VR headsets are now as ubiquitous at Windsor University School of Medicine as stethoscopes. Students participate in what the university refers to as “immersive rotations.” They conduct surgeries, diagnose virtual patients, and even handle unforeseen emergencies using intricate simulations. It’s especially helpful for boosting self-esteem prior to clinical exposure. Every scenario, such as a patient’s worried look, a nurse’s urgent voice, or the faint panic in a busy emergency room, is meticulously designed to replicate emotional realism.
| Category | Information |
|---|---|
| Core Concept | Virtual Reality (VR) creates immersive, interactive environments where medical students practice procedures safely and realistically |
| Key Innovators | Harvard Medical School, Stanford Medicine, Windsor University School of Medicine |
| Leading Researchers | Dr. Justin Pottle (NIH), Dr. M. Mergen (BMC Medical Education), Dr. G. Lampropoulos (MDPI) |
| Core Benefits | Safe simulation-based learning, improved anatomy visualization, empathy training, and risk-free procedural practice |
| Key Technologies | VR headsets, 3D anatomical mapping, AI-integrated diagnostics, haptic feedback gloves |
| Institutional Adopters | Mayo Clinic, Johns Hopkins, Oxford, and Windsor University School of Medicine |
| Primary Impact | Enhances medical training accessibility and boosts student confidence and skill retention |
| Industry Trend | Increasing use of VR for surgery, diagnosis, and patient empathy simulations |
| Global Perspective | VR bridges resource gaps in developing countries through affordable, remote medical training |
| Reference Source | https://www.windsor.edu/virtual-reality-in-medical-education |
For educators, virtual reality is a pedagogical innovation rather than a new technology. It closes the intimidating gap between practice and knowledge. Before ever entering a hospital, a student can complete dozens of virtual surgeries, and each repetition improves accuracy and memory. The approach is very effective, lowering first-year students’ anxiety levels while saving time and money.
Another intriguing layer is empathy, which is highlighted by MDPI’s Dr. G. Lampropoulos. Students can experience chronic pain, dementia, or visual impairments by using virtual reality to put them in the shoes of patients. It has a profoundly humanizing emotional impact. In one dementia awareness simulation, students are left feeling lost in a hospital hallway and unable to remember their location. Future medical professionals are not only technically skilled but also emotionally sensitive, two qualities that medicine sorely lacks.
One of VR’s most well-known applications is for surgical simulations. With haptic feedback that simulates texture and resistance, platforms such as Touch Surgery and Osso VR replicate actual procedures. The ability of surgeons to virtually practice intricate procedures has significantly increased accuracy and decreased intraoperative errors. These instruments are now essential components of contemporary surgical preparation for medical facilities like Johns Hopkins and the Mayo Clinic.
The economic ramifications are just as striking. Expensive cadavers, lab equipment, and physical spaces are necessary for traditional medical training. After the initial investment, virtual setups, on the other hand, are surprisingly inexpensive. Due to logistical and geographic constraints, universities are able to train hundreds of students at once. This invention is especially revolutionary for developing nations with limited access to cadavers.
Virtual reality is also being used to reinvent medical residency programs. Rare operations like heart transplants and neurosurgical procedures are now virtually practiced by Stanford Medicine residents. In addition to being much quicker, the training is safer, guaranteeing that young physicians approach actual surgeries with comfort and familiarity rather than fear.
VR is changing the way compassion is taught outside of the classroom. Medical students can participate in a program at Oxford that simulates what it would be like for a patient to receive a terminal diagnosis. Empathy is developed via lived experience rather than theory in this emotional journey. According to an Oxford instructor, “you can’t teach compassion through slides, but you can make someone feel it through simulation.” The exercise is very good at developing bedside manners, which is something that is frequently neglected in conventional training.
It’s interesting to note that celebrities are also contributing to this change. Through Sound Ventures, his venture capital firm, Ashton Kutcher has made investments in VR healthcare startups that specialize in medical education. In an effort to enhance empathy and communication, Serena Williams has sponsored immersive programs for pediatric physicians. Despite being unexpected, their participation is indicative of a growing social conviction that technology, medicine, and empathy must all advance simultaneously.
According to Windsor University, students who trained in anatomy using virtual reality (VR) did noticeably better on written and clinical tests. Unlike those trained with 2D models, they were able to recall spatial orientation and structural relationships with remarkable clarity. In contrast to traditional study methods, the tactile experience of manipulating organs—even virtually—created memory pathways.
Furthermore, continuous self-evaluation is guaranteed by the feedback mechanism incorporated into VR systems. Pupils’ performance is evaluated in real time according to timeliness, accuracy, and procedural flow. It’s a personalized, data-driven education. Every action, no matter how good or bad, becomes a teaching moment. The process is significantly better than static demonstrations because of this continuous feedback loop as well as the pause, rewind, and replay features.
It is impossible to overestimate VR education’s global reach. A student in Kenya can join peers in Boston or London in a virtual operating room via virtual reality networks. They converse, share ideas, and practice techniques at the same time. Medicine becomes more collaborative and inclusive as a result of this connectivity. It’s democratizing knowledge across national boundaries, which was previously unthinkable.
AI and virtual reality are also being combined in medical facilities. AI-powered simulations examine performance patterns, identify vulnerabilities, and dynamically adjust difficulty levels. Particularly creative is this hybrid approach, which produces individualized learning paths with no two sessions being the same. Training thus becomes highly adaptable, reflecting the unpredictability of actual medical practice.
