In the first week of February, Singapore reported two new cases of measles, increasing the country’s total for 2026 to 13. Although the number is low, it is very comparable to the pattern observed in prior years when early containment was required due to small clusters.
The 13 cases already exceed the total number of 2024 cases and are over half of the 27 annual cases in 2025. Health officials are responding with noticeably increased vigilance, anxious to stop minor sparks from spreading, even though the numbers are still well below the 152 occurrences recorded in 2019.
Two infections were found between February 1 and February 7, compared to five the week before. Instead of momentum, that variation points to movement. Such modest changes can be especially instructive in epidemiology, directing treatments before transmission solidifies.
The Communicable Diseases Agency of Singapore has taken prompt action.
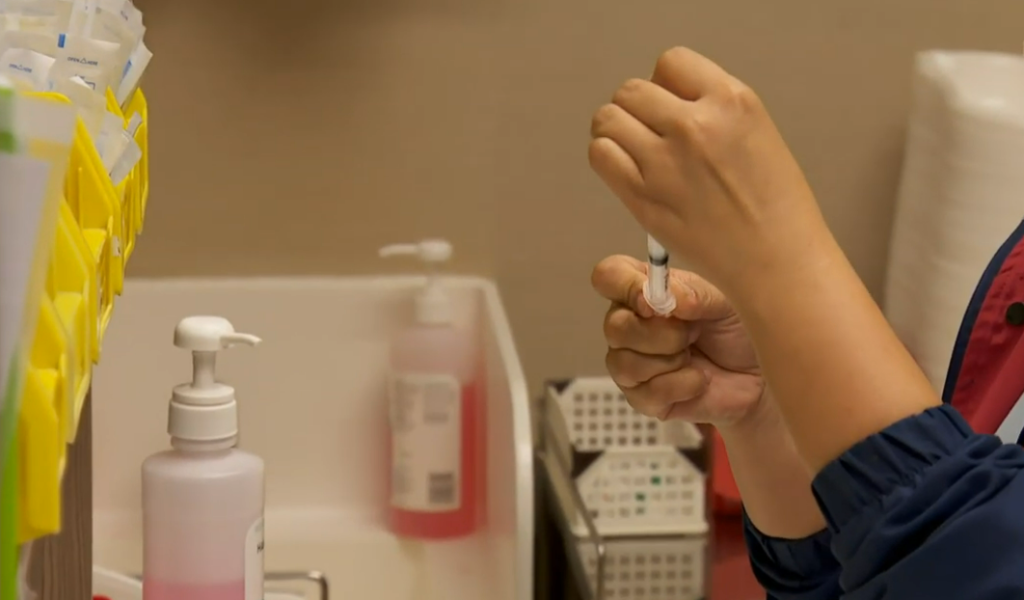
Confirmed patients are now subject to mandatory isolation until they are no longer contagious. Close contacts without immunity are required to be vaccinated or to remain in quarantine at home for a maximum of 21 days. These actions might seem ordinary, but when taken early on, they are incredibly powerful instruments.
Measles can stay in the air for up to two hours and is spread by respiratory droplets. Even though most patients recover in a few weeks, complications like pneumonia or encephalitis still pose a major risk, particularly for young children. Frequent symptoms include fever, cough, sore throat, and rash.
| Key Context | Details |
|---|---|
| Country | Singapore |
| New Cases (Feb 1–7) | 2 |
| Total Cases in 2026 (as of mid-February) | 13 |
| Cases in January 2026 | 11 |
| Cases in 2025 | 27 |
| Major Historical Spike | 152 cases in 2019 |
| Agency Involved | Communicable Diseases Agency (CDA) |
| Key Measures | Mandatory isolation, contact tracing, quarantine up to 21 days |
| Childcare Centres | No confirmed cases as of Feb 12, 12pm |
The best defense is still vaccination.
Up to 97 percent immunity can be obtained with two doses of the MMR vaccination, given at 12 and 15 months. That protection has greatly decreased the chance of long-lasting epidemics in a nation with continuously high vaccination rates.
Mobility, however, puts even robust systems to the test.
Measles cases in Singapore during the last 10 years have frequently been the result of imported illnesses connected to international travel. Small pockets of vulnerability can be found by a cross-border virus, especially in people whose immunity has weakened or who have postponed vaccination.
The January report contained one noteworthy detail. Despite having no documented interaction with one another, three individuals were infected with genetically linked virus strains, which may indicate undiscovered community transmission. Even in cities with comprehensive health records, invisible chains can quickly form, as I was quietly reminded when I read it.
The agency’s reaction to tracing and isolation has not been restricted.
For a scalable health surveillance service provider that could start contact center operations in less than a day, a tender was issued. Such infrastructure could handle thousands of calls and texts per day at full capacity, demonstrating a considerable improvement in preparation since expenditures made during the pandemic.
These days, technology is essential.
Random video-call inspections aid in ensuring that quarantine and home isolation regulations are followed. Authorities have created a very effective monitoring system that strikes a balance between enforcement and pragmatism by utilizing digital tools and systematic follow-ups.
Communication has become just as crucial as containment tactics.
Parents were alarmed by the widespread online rumors regarding diseases at daycare facilities. In response, the organization made it very clear that, as of midday on February 12, there were no confirmed instances of measles in preschools or daycare facilities. All of the suspected instances that the doctors had referred had tested negative.
That explanation was really helpful in preserving confidence.
Speculation may spread quickly in closely knit communities—sometimes even more quickly than viruses. An entire neighborhood’s level of worry can be increased by a single social media post. Prompt and clear communication helps prevent anxiety from overriding the facts.
The existing state of affairs is not a crisis.
Even though there are already 13 cases, which is more than there were last year, they are still under control. In order to drastically lower the possibility of a wider spread, enhanced methods are intended to guarantee that transmission chains are interrupted quickly.
Public health responses changed during the epidemic as millions of people worldwide used remote work and digital surveillance tools as standard practices. Lessons learnt during that time are reflected in Singapore’s current measles strategy, which streamlines procedures and frees up human talent for focused epidemiological work.
Rather of being dramatic, the pace seems routine.
Regular health bulletins are issued. The rules of isolation are discussed in detail. Tracing contacts happens in silence. The cadence of the system’s operation is constant and seems to be quite dependable.
However, uneasiness persists in subtle ways.
Parents remember previous surges. Medical professionals continue to pay attention to rashes that may have appeared commonplace in the past. Memories of previous outbreaks can be evoked by even slight increases in the number of cases.
Being ready is the motivating factor.
Singapore has developed a very adaptable system by combining vaccine policy, quick tracing, digital monitoring, and public communication. It instantly adjusts, easing when trends stabilize and scaling up as needed.
Timing is critical for early-stage clusters.
In terms of preventing further spread, swift separation is especially creative. Non-immune contact quarantine serves as a barrier, allowing epidemiological research to elucidate the routes of transmission.
High vaccination rates have significantly increased community resilience over the last ten years. Resilience greatly lowers the likelihood of widespread epidemics, but it does not completely remove risk.
Singapore’s February numbers are not a warning, but a reminder.
