It was a Tuesday afternoon, and the waiting room was unusually quiet. Wearing a wrinkled office shirt and running shoes, the young man sat scrolling through his phone, looking more like he was waiting for test results than a dental cleaning. He was no more than thirty years old. As events like these take place, it seems as though something has changed with regard to cancer, subtly moving into an age group that was previously shielded by youth.
As a diagnosis linked to retirement years, grey hair, and accumulated time, cancer was largely relegated to the background of older adulthood for decades. Now, however, physicians are noticing something that causes them to pause. early onset of tumors. diagnoses in people who are starting their careers, purchasing homes, or preparing to start a family. Although the precise cause of the current shift is still unknown, lifestyle choices appear to play a role.
| Key Information | Details |
|---|---|
| Health Trend | Rising early-onset cancer diagnoses in adults under 50 |
| Most Affected Age Group | Adults in their 20s and 30s |
| Major Lifestyle Factor #1 | Diet high in processed foods, low in fiber |
| Major Lifestyle Factor #2 | Sedentary lifestyle and lack of physical activity |
| Most Linked Cancer Types | Colorectal, breast, uterine, pancreatic cancers |
| Global Health Authority | National Institutes of Health Study |
| Cancer Research Insights | Cancer Research Institute Analysis |
Dietary suspicion is among the most unsettling. Convenience and speed have shaped modern eating habits, which frequently center on processed foods. Every supermarket has entire aisles devoted to products that are meant to last for months. Vibrant packaging. lengthy lists of ingredients. These foods, which are high in sugar and additives and low in fiber, may be subtly altering the way the body works.
Previously found naturally in fresh foods, grains, and vegetables, fiber now frequently feels optional. The digestive system acts differently in its absence. Inflammation may persist. The bacteria in the gut change. According to doctors, this environment might foster circumstances that could lead to tumors developing earlier than anticipated. It seems that even after years, the body retains the information it has been given.
The act of moving has also become less frequent. It used to be necessary to walk between offices or buildings. Whole days now pass in a chair. During meetings, meals, and entertainment, people sit, sometimes standing for hours at a time. Late into the night, screens glow, keeping muscles motionless and bodies awake.
It’s difficult to ignore how commonplace this has become. Sitting is not thought to be harmful. It is regarded as fruitful.
However, sedentary lifestyles are increasingly linked by researchers to an increased risk of cancer. Weight, hormone levels, and metabolism are all impacted by physical inactivity. These internal alterations may eventually promote the growth of tumors. The speed at which this process occurs and the reasons why some people are impacted while others are not are still unknown.
A change in culture is also at work. Work has become less physically active but more mentally taxing. Faster food has become less nutritious. Stress has decreased in visibility but has become constant. On its own, each element might appear controllable. When combined, they create a pattern from which it is challenging to break.
Because colorectal cancer is becoming more common in those under 40, doctors are particularly concerned about it. Sometimes the symptoms of these cases are disregarded, leading to a delayed diagnosis. Fatigue turns into “burnout.” Discomfort with digestion turns into “stress.” The notion that youth equates to health persists for longer than it ought to. The ease with which warning signs can be incorporated into daily life is unnerving.
Another layer is added by obesity, which is strongly linked to both poor diet and inactivity. Insulin levels, inflammation, and hormone balance are all impacted by excess weight. These changes don’t make a big show of themselves. They develop gradually over years, frequently going unnoticed.
The extent to which contemporary lifestyles alone account for the increase is still unknown. Roles include genetics, exposure to the environment, and enhanced detection. However, a lot of medical professionals think it’s impossible to overlook lifestyle changes.
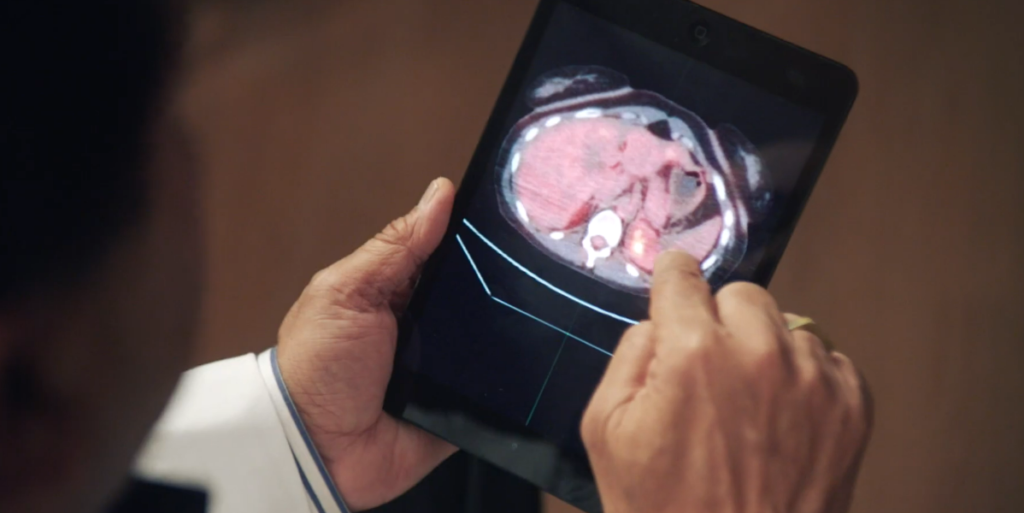
The atmosphere changes when you see younger patients entering oncology clinics. These are people who anticipated facing death decades in advance. Their presence makes the illness feel closer and less distant.
There is cautious optimism at the same time. Lifestyle choices are subject to change, unlike genetic factors. Diet can get better. It is possible for movement to return. Future risk may be altered by small choices made repeatedly over many years.
However, those choices are rarely encouraged in modern life. Time is saved by fast food. Desk work pays well. Screens provide endless entertainment.
But it might take years before the cost is apparent.
In research facilities and hospitals, a silent realization is beginning to take shape. Cancer is no longer patiently waiting for old age to strike.
