One of the most reliable treatments for potentially fatal bacterial infections is daptomycin, an exceptionally potent antibiotic known for its accuracy and speed. This product, which comes from Streptomyces roseosporus, is the ideal fusion of natural origin and scientific advancement. Due to its ability to precisely target harmful bacteria while preserving the body’s healthy systems, doctors refer to it as “the antibiotic that thinks.” When antibiotic resistance started to overwhelm conventional treatments, particularly against MRSA and VRE, its discovery—which had been buried for decades in pharmaceutical archives—resurfaced.
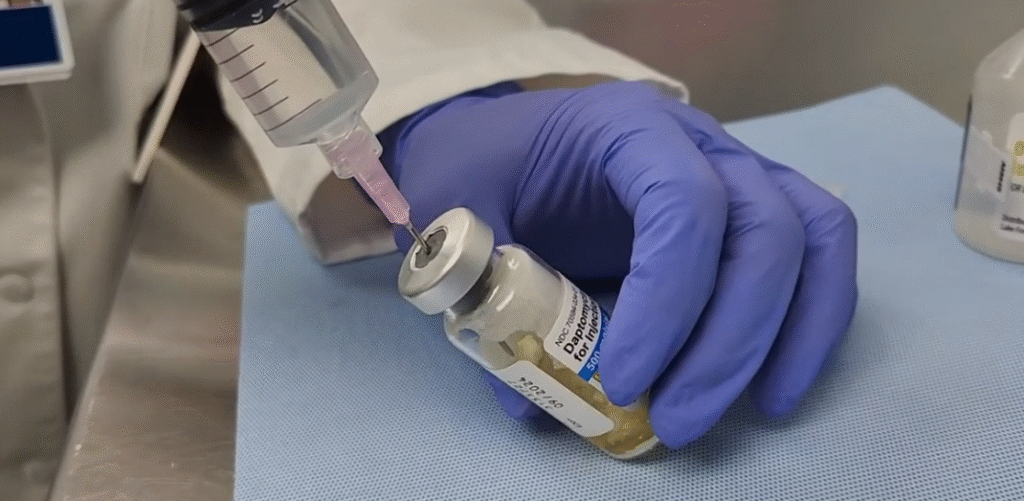
This antibiotic disrupts essential cell functions in a calcium-dependent manner by slipping its lipophilic tail into bacterial membranes like a key into a lock. Bacterial membranes break down in a matter of minutes, thereby halting the synthesis of proteins, DNA, and RNA. In addition to being quick, this technique is very effective; a single infusion can reverse the course of severe infections that previously seemed incurable. Its science is very clear, showing that targeted chemistry can work better than pharmaceutical force.
In situations where bacterial resistance can be lethal, such as bloodstream infections and right-sided infective endocarditis, clinicians believe that daptomycin is especially helpful. Daptomycin was the next line of defense when the older antibiotic vancomycin started to lose its effectiveness. It is focused, quick, and devastatingly effective against its targets, much like a specialized rescue team that shows up when all others have failed.
Table: Key Facts about Daptomycin
| Category | Details |
|---|---|
| Drug Name | Daptomycin |
| Brand Names | Cubicin, Cubicin RF, Dapzura RT |
| Drug Class | Cyclic lipopeptide antibiotic |
| Manufacturer | Originally developed by Eli Lilly; now marketed by Merck & Co. |
| Approved Uses | Complicated skin infections, MRSA bacteremia, right-sided infective endocarditis |
| Mechanism | Disrupts bacterial cell membrane through calcium-dependent binding |
| Major Targets | MRSA (Methicillin-resistant Staphylococcus aureus), VRE (Vancomycin-resistant Enterococci) |
| Not Used For | Pneumonia (inactivated by lung surfactant) |
| Common Side Effects | Muscle pain, headache, insomnia, diarrhea, injection-site reactions |
| Monitoring | Weekly creatine phosphokinase (CPK) levels during therapy |
| Reference | Mayo Clinic – Daptomycin Overview |
Its one drawback, however, is that it cannot treat pneumonia due to a peculiarity in science: the drug loses its effectiveness when it comes into contact with the surfactant that coats lung tissues. To get around this obstacle, researchers from several important institutes are creating new derivatives. This goal demonstrates how science can continue to innovate under pressure and reflects a resurgence of confidence in antibiotic innovation on a global scale.
The drug’s comeback also signaled a shift in antibiotic stewardship, the field of medicine that aims to use these potent substances sensibly. Experts in infectious diseases stress that each dose of daptomycin serves two purposes: healing and preserving future efficacy. Strict usage guidelines have been implemented by hospitals, which have reported markedly better patient outcomes, lower resistance rates, and noticeably quicker recovery times.
The story of Daptomycin is intriguing in part because of its strange beginning. It was found in a soil bacterium decades ago, but formulation issues caused it to be shelved. Researchers dusted off those early findings and redesigned them for contemporary use when superbugs started to outperform older medications. Cubicin, a reintroduction that offered hope, was the outcome. Its reintroduction into clinical practice was not a coincidence; rather, it served as a reminder that revisiting lost discoveries is frequently necessary for advancement.
There are lessons to be learned from the drug’s mechanism that go beyond medicine. It changed the way scientists create therapies for resistant pathogens by emphasizing the disruption of bacterial membranes rather than the disruption of their growth cycle. New antibiotic generations have been inspired by this strategy, which has established a standard for more intelligent molecular design. Similar to how renewable energy changed conversations about sustainability, this scientific advancement has subtly changed the pharmaceutical industry.
This scientific tale also has an unexpected human component. Daptomycin, a drug that succeeds where others fail, can feel like a second chance for patients suffering from MRSA or bloodstream infections. Hospital infectious disease specialists frequently describe instances in which patients who were once critically ill recovered quickly after starting Daptomycin treatment. These findings highlight its emotional resonance as well as its pharmacological potency, making it a representation of resiliency in contemporary medicine.
An important point of caution is the antibiotic’s interaction with statin medications. In order to prevent muscle damage, doctors typically stop cholesterol treatments while Daptomycin therapy is being administered because both can strain muscle fibers. Weekly CPK monitoring guarantees early detection of even minor side effects. This meticulous oversight demonstrates how precision medicine has changed, becoming proactive rather than reactive in order to foresee issues before they become more serious.
As a reflection of modern medicine’s preference for individualization over generalization, pediatric and elderly patients require customized dosage. While older people with slower kidney function may require adjusted intervals, younger patients metabolize it more quickly. This careful personalization shows how far contemporary care has advanced, striking a striking balance between effectiveness and empathy.
Public health programs in the United States and Europe have begun incorporating daptomycin into more comprehensive antimicrobial resistance strategies. In order to create next-generation formulations that combine Daptomycin with linezolid or ceftaroline and produce synergistic effects, the NIH and pharmaceutical companies have formed research partnerships. These partnerships are especially creative, demonstrating how cross-sector collaboration can lead to innovations.
Daptomycin has come to represent scientific tenacity in cultural discourse. Researchers and patients alike are reminded by its tale that nature frequently conceals answers in plain sight. The soil-borne origin of the compound seems almost poetic—a natural defense mechanism that has been transformed into a treatment that can save lives. The finding supports a broader notion that progress can sometimes be achieved by seeing the potential in what already exists rather than by inventing something new.
The effectiveness of daptomycin has had an economic impact on the healthcare sector as well. Hospitals report lower healthcare costs due to shorter stays, fewer relapses, and less need for secondary therapies. Daptomycin has proven to be both medically and financially indispensable by expediting patient recovery and reducing complications. Because of these two advantages, it is especially advantageous for healthcare systems that are under pressure from chronic infections and financial limitations.
